The Dietrich/Mulder/Gerke orthopedic/anesthesia team spent April 19 – 24, 2015 at Hopital Adventiste d’Haiti (HAH) and the following is their report. Terry and Jeannie Dietrich have established the Dietrich Haiti Indigent Patient Fund through Amistad International to create an endowment that will sustain itself to facilitate patients who don’t have the means to pay for life-changing surgeries.
The OR remodel project a HAH is not finished however the new hospital administrator, Ed Martin, and Scott Nelson encouraged us to take a team to the hospital. It is especially important to continue to support Francel and the orthopedic program. Our planned trip 6 months ago was suspended at the request of Mr Martin due to the financial and staffing issues he was struggling with at the time. Fortunately a semblance of stability has been regained.
Francel Alexis is a young Haitian orthopedic surgeon. He was born and raised in Le Caye on the south coast. It is about a 4-5 hour drive from Port as Prince. He did an orthopedic residency in Haiti. Scott first told me about him in 2011 when he was doing a pediatric orthopedic residency at the CURE hospital in Santo Domingo. Dr Alexis had been planning to return to his home town to practice pediatric orthopedics. Scott thought he might be a good candidate to work and perhaps even be in charge of the orthopedic program at HAH. We contacted him and his CURE sponsors and arranged for him to spent the last several months of his fellowship at HAH with me. He would also be able to learn pediatric orthopedics from Scott and the other orthopedic teams coming to HAH. At our encouragement, he has stayed to work at HAH. He has been a great addition to the orthopedic work at HAH. We continue to sponsor him and support him with expertise, and orthopedic materials, supplies, equipment and implants. I contacted Francel and requested that he find as many patients as possible for arthroscopy. He made good progress with his arthroscopy skills during our last trip here in April of 2014. Our plan was to build on that experience and help him to reach a new level of comfort and skill doing arthroscopy.
The new administration of HAH headed by Ed Martin has been tasked with paring down the hospital staff. Many workers have been laid off in this challenging time since the loss of the Embassy clinic. Additional challenges continue to present themselves. Slow but steady progress seems to be occurring. The plan still continues to be for the hospital to be financially stable with all overhead covered by the paying patients. Then the “true costs” for the additional nonpaying patients will be minimized with the visiting teams bringing disposables, medications, supplies and implants. There is even hope the Embassy contract might be regained. The Emergency Room is currently located in the area where the Embassy clinic was held.
Volunteer housing for the visiting teams remains in the small building just below the rehab center. Some good changes have been made. The 6 bunk beds have been replaced with 6 single beds. Obviously, this change limits the number of volunteers able to stay on the hospital compound. A second small table has been added as well as a small couch. The biggest and nicest change is the kitchen sink and counter with cabinets. Now we have adequate space for food preparation and clean up. The tasty meal provided daily of rice, beans, vegetables and salad has been nearly twice as much as the four of us can eat. The internet connection is pretty good although a bit slow. I was able to use the internet most of the time but Tim never got it to work. The small air conditioner cannot keep up with the heat generated by the Haitian midday sun. We are only there for brief periods at that time of day so it doesn’t really matter much. It is plenty cool at night and in the morning. Two strong oscillating fans keep the air moving. Jeannie made nice curtains for all of the windows at Scott’s request. They look very nice. Jeannie also brought nice sheets and blankets for each of the beds. It is beginning to look and feel much more homey. The afternoon sun hits the side and roof of the building directly. The idea occurred to us that shade would keep the house cooler and use less energy in the process. Steve generously paid for a nice grafted mango tree. If it grows fast, it will be making shade in a couple of years. The fruit will be an added benefit.

- Tim Gerke and Steve Mulder, the anesthesia team, using ultrasound on the right to administer a nerve block
Our Anesthesia providers for this trip to HAH consisted of Dr Steve Mulder and Tim Gerke student CRNA. Tim is our son-in-law. He and our daughter ,Summer, live in Portland Oregon. Tim has about 8 months left in his 27 month training program. He has already completed 3 ½ months of clinical rotations. Dr Mulder is a graduate of the Loma Linda University School of Medicine. He has been practicing anesthesiology nearly 30 years in Central California since finishing his residency training. This was Steve’s seventh trip to Haiti, all since the earthquake. He is an excellent specialist. He is well acquainted with the challenges of providing high quality anesthesia in a third world country. The anesthesia machines do not receive regular servicing. The ventilator was missing from the machine in OR #2. Reliable pediatric laryngoscopes were hard to find. The normally used supplies were missing or hard to find in the anesthesia carts. The touniquet pressure control alarm continuously sounded its high pitched beep. Heart sounds were nearly impossible to hear especially when combined with the racket from the suction device. Muffling both of those very loud sounds provided partial relief. Our temporary OR situation at HAH does not give us space for anesthetic recovery. Both Steve and Tim kept very positive attitudes and continued giving excellent anesthesia in spite of these challenges. They both have such a heart for this type of work. Their wives, Victoria and Summer, deserve lots of kudos for their willingness to let their husbands come to Haiti without them.
Tim arranged with the Sonosite Company to let us use an ultrasound unit during this trip. Many of our patients, large and small, were able to get a regional or nerve block. Post operative pain control is much easier. Many patients awakened from the anesthesia with little or no pain. The general anesthetic used is almost always much lighter and there is less or even no postoperative nausea. The immediate post op recovery is also much smoother with much less respiratory depression.
I had arranged for Francel to bring as many patients as possible with knee and shoulder problems so that we could focus on him learning arthroscopy. The first several cases took longer and he was somewhat more tentative. Movements didn’t seem very confident and at times seemed somewhat counterproductive. With more time and as more cases were done there was a clear improvement in the ability to obtain good visualization. Movements were much more confident. His ability to place instruments in the visualized areas improved significantly. I am sure that Francel will now start doing arthroscopy cases on his own and progressively improve as time goes on. A vigorous sportsmedicine/arthroscopy program would undoubtedly be beneficial to both the hospital as well as Francel. Almost all of the patients are outpatients. They use few hospital resources. None of the other local orthopedic surgeons do any significant arthroscopy. A strong program here will not have a negative impact on their practices. It is conceivable that patients with ability to pay could be attracted to HAH. This could help Francel’s private practice to grow. It could also help to stabilize the hospital financially.
James Jean Baptiste is an orthopedic surgeon who is a good friend of Francel’s. He works for Doctors Without Borders here in the city. They studied together through med school and residency training here in Port au Prince. He came several days to learn as much as possible. He scrubbed with us on some of the arthroscopy cases. He has a strong desire to learn arthroscopy skills. He might be a very good candidate.
Dr Eldine Jacques is a young colleague of Francel’s. She is a bit younger than him. She did a fellowship in Pediatric Orthopedics and currently is the orthopedic director for CURE in Haiti. She is in charge of the clubfoot program. She does all of her surgical cases at HAH. She is very likable, has a beautiful smile and adds a real touch of class to the whole program.
JJ, Emmanuel, Roosevelt and Joseph are four of the original translators that we have maintained fairly close contact with since we left after our year volunteering at HAH. We had a closer relationship with them because they frequently would accompany us on the occasional trip away from the hospital. We went to Jacmel on a couple of occasions. We went above Petionville to Fermathe more than once. We even made it all the way to Furcy one time. Roosevelt came with us when I arranged for us to go on a boat ride in a “cannot” to the Acardin Islands. That was an amazing day. We had a great time looking for shells, eating our picnic lunch and then getting great photos of the whole experience including the homemade boat and sails and our captain. JJ, Emmanuel and Roosevelt came with me on our long weekend trip to Mirabalais and then down the Artibonite valley to Molina sur Mer resort. We had a great time hanging out and enjoying the pool, beach and other amenities of the resort. None of the three had ever been to a resort before.
All of them are doing very well. JJ and Roosevelt have finished with at least the first phases of their training and are working at the hospital. Roosevelt is a PT tech and really is enjoying his work. Emmanuel continues to organize and run the ortho clinics. He remembers the patients very well and communicates with them frequently. He is still studying business. He would like to eventually work as a hospital administrator. Joseph Rika is nearing the end of his PT tech program. JJ, Emmanuel, Elaine and others planned a great evening at the Auberge. We celebrated Jeannie’s 33rd birthday by stuffing ourselves with pizza and birthday cake. It was a great evening.
Elaine Lewis is an amazing person and is doing a remarkable job. Her life journey has brought her to HAH as a volunteer for at least 6 months. After more than 30 years working as a homemaker and caring for her husband and their seven children she started working part time teaching English as a second language. A lifelong desire to participate in overseas medical mission work led to a training program as a surgical tech. Providentially she found haitbones.org and contacted Dr Scott Nelson. Arrangements were made for her to come to HAH and use her organizational and teaching skills. Fortunately she was able to convince her husband, Jeff, to take a sabbatical from his teaching responsibilities as an assistant professor of Intercultural Studies at California Baptist University.
The ongoing delay in the OR remodel has now given Elaine the challenge of making the temporary ORs as clean, organized and efficient as possible. Identifying the employees that are suited to the operating room is key and training those that are a good fit is essential. She has clearly identified JJ as highly trained and motivated. He understands the orthopedic equipment and setup much better than anyone else and is also doing a remarkable job.
The C-arm image intensifier is absolutely indispensible for doing high quality orthopedic surgery. Our OEC has been worth its weight in gold. It was donated through the generosity of several American orthopedic surgeons shortly after the earthquake. For more than 5 years it has served the visiting orthopedists faithfully for the most part at HAH. On a couple of occasions the screen gave us an “ERROR” message and we were left hanging. One of those incidents led to a 45 minute phone call to the OEC tech in Salt Lake City. Scott in his inimitable fashion boldly disassembled parts of the unit to gain access to the “potentiometer.” That particular item has a touchy adjustment. A new potentiometer and some fine tuning later, it started to work again. Current fluctuations which are daily if not hourly occurrences in Haiti probably were the cause. Keeping the unit always plugged into the invertor circuit protected all of our electronics including the C-arm from those fluctuations.
The OR crew knows that the C-arm must be handled carefully so that it doesn’t hit walls or other obstacles when it is being moved. The old ORs had an irregularity in the tile floor that made it difficult to move the C-arm from room to room easily. The temporary OR floor is smooth allowing easy movement of the C-arm. We were able to use it in both rooms and even the hallway without any issues this trip. I am confident that the new ORs will have perfectly smooth floors. They are nearly done with only the last couple of rows of tiles to be laid at the very entrance to the OR suite. The C-arm worked without a single hiccup this trip. It must be the grace of God that has protected it from the power issues for the last year while we have been in the temporary OR. The Fuji digital xray machine had not been working for about 2 months. That placed a bigger burden on the C-arm which was used a lot more to keep the costs down for the patients unable to pay. A tech from Fuji repaired it last week and it worked better than ever during our week.
The OR suite remodeling project is making slow, agonizingly slow, progress. It has promise to be an exceptional facility, possibly the best in the country. The entire rewiring and control panel in the shop area under the ORs is certainly an impressive change from the preexisting ratsnest of wires that were clearly very dangerous. The air exchange system that is essential for a good environment that will be acceptable for joint replacements has also been installed. Scott included pictures of the units in his latest blogpost. Major dollars must have been spent to accomplish both of those feats. The three ORs are currently getting the overhead lights installed. (WHAT? No more headlamps?) The designated area for post anesthesia recovery looks very nice. I am excited along with everyone else for the project to be finished.
The current temporary OR is just that. It occupies the natural space of the emergency room. I am writing this in the back storage area and am being attacked by hordes of tiny ants. They chase across my computer screen randomly. Not a day has passed that mosquitoes have not been flying through our sterile fields. The flies have yet to invade which is good. The job of organizing the ortho equipment, implants and surgical supplies has been done in an outstanding fashion by Elaine, JJ and Scott and his team. The C-arm is running beautifully (knock on wood.) The printer even works nicely now that it was discovered to have the paper roll wrongly inserted. We utilized the smaller OR for several of our cases. Even when we needed the C-arm, we were able to get it far enough into the small room to xray the part being operated on. Of course, the monitor had to remain in the hall. A bit inconvenient, but it works.
We had a great mix of patients. The prior problem of patients being signed up for surgery but then not showing up after their interview with administration seems to have been solved. We had no “no-shows.”
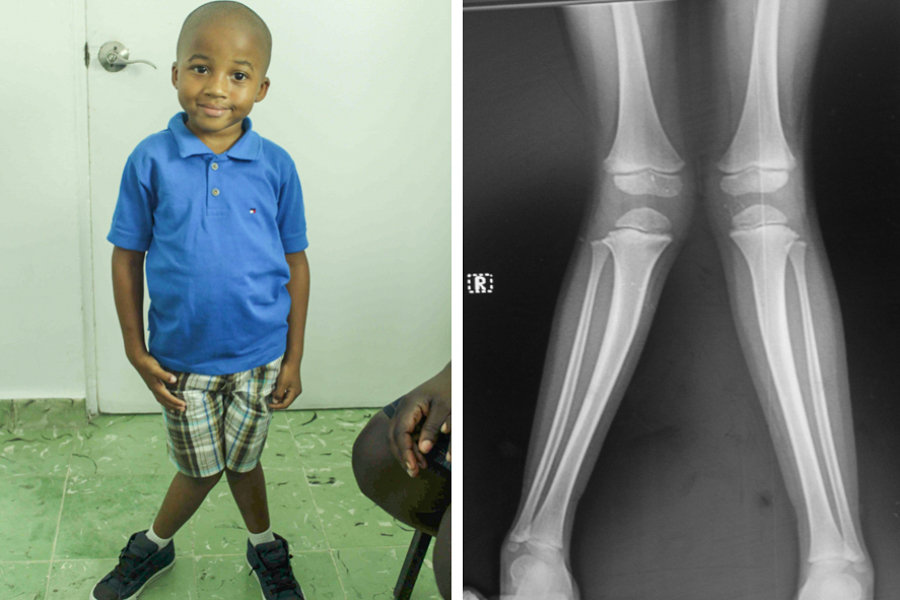
Aside from the arthroscopies, we did nearly 20 other cases during our 4 days of operating. Several kids with genu valgum and varum got 8-plates. An older teenager had closed epiphyses and got a femoral osteotomy and Orthofix. A 30 y/o had a large mass on the plantar surface of her foot measuring 8×6 cm. Previous biopsy at the General Hospital had showed it to be a hemangioma. Complete excision with wound closure was possible.
While I was busy with the foot tumor, Francel and James did an IM rod removal from a patient with a malunited (30 degrees of ext rotation) femur fracture. He did a derotation osteotomy and fixed it with a locked SIGN nail. A patient with a dislocated patella came for surgery. She had had a prior patellar tendon advancement and proximal realignment for “patella alta”. It had obviously not stabilized the patella sufficiently. She had not had recent trauma. I did an aggressive open lateral release, medial plication, VMO advancement and distal realignment with a Roux-Goldthwait procedure. The patella was very stable when the case was finished and the knee flexed easily to 130 degrees. I also did a patellar nonunion. The trauma occurred 7 months ago. The open reduction and Fig 8 tension band wiring went well.
My last case was a patient injured in the earthquake Jan 12, 2010. She sustained an open tibial fracture from a crush injury. Three operation later she was “free” of infection. The tibia finally healed as well. 4 days ago, she had a sudden spontaneous pain in her mid/distal tibia. The entire middistal pretibial area was very tender and swollen. She was febrile. The xray was very suspicious for a small middistal tibial sequestrum. Clinically the infection had flared up. The incision released more than a half cup of pus under pressure. The 15 centimeter window in the tibia showed a sinus leading to a fairly small sequestrum. The thorough debridement, washout and antibiotics may perhaps cure her. It wouldn’t be surprising though if more similar events will occur in the future. It is not uncommon for this type of bone infection to be a lifetime condition.
A major problem surfaced when we did a case with plans to place a wound vac. We were unable to use any of them as they all required an “access code” to be activated. All efforts to put them in use were stymied. Many calls to LLU and to the company could not solve the problem. We are going to try to reconnect with Jan a nurse from SanDiego who is a vac specialist. She solved a similar problem for us several years ago on our first trip to HAH.
Overall, this trip was one of the best for Jeannie and me of our seven weeklong trips to HAH. Much can be attributed to Francel and his hard work. He relates very well with patients and gets along very well with hospital workers, administration and volunteer team members. His progress in learning arthroscopy is really exciting to me. The two young orthopedists that are working with him can add strength to the program. The equipment, with the exception of the vacs, was all in good working order. The temporary ORs are adequate although incapable of being sealed to prevent insect invasions. It is exciting to see the OR remodeling project well on its way to completion. JJ now has formal training to give him credibility as a health care worker. Elaine’s hard work and contributions have been priceless. With God’s continued blessings, HAH will continue to provide excellent orthopedic care to all Haitians regardless of their ability to reimburse the hospital for the services rendered.
Discover more from haitibones
Subscribe to get the latest posts sent to your email.














Recent Comments